News
First Stage Stem Cell Trials Show Promising Results for Type 1 Diabetes Sufferers
23/05/2018
A new bioengineering processes called self-condensation cell culture is using stem cells to successfully treat type one diabetes in primary trials.
The new trial is a breakthrough for medical science, pushing medical professionals closer to one day being able to grow human organ tissue from their own stem cells for regenerative therapy say study investigators at Cincinnati Children’s Hospital Medical Centre in the U.S. and Yokohama City University (YCU) in Japan.
This means that when these studies use a patient’s own stem cells, instead of a donor, they are an automatic match, so there is less chance of the new stem cells or organ to be rejected.
Within the UK, 4 million people have diabetes, which is the same as one in every 16 people.
Diabetes is caused by defective beta cells in your pancreas, meaning that a person with type 1 diabetes cannot processes sugar properly.
This means that a person suffering from this type of diabetes can have their sugar levels plummet or rises quickly, which can be detrimental to a person’s health if it isn’t medicated properly.
This new treatment, in the first trail stages, hopes to eventually cure diabetes, so there is no need for an epi-pen. The patient would be given synthesised artificial cells (from stem cells) which would act as effective beta cells.
Takanori Takebe, MD, a physician-scientist at the Cincinnati Children’s Centre for Stem Cell and Organoid Medicine, said: “This method may serve as a principal curative strategy for treating type 1 diabetes, of which there are 79,000 new diagnoses per year,”
“This is a life-threatening disease that never goes away, so developing effective and possibly permanent therapeutic approaches would help millions of children and adults around the world.”
Takebe, who has a dual appointment in the Department of Regenerative Medicine at YCU, highlighted that the technology would need additional research before it can be used therapeutically in a clinic. He is the study’s co-lead investigator along with YCU colleague, Hideki Taniguchi, MD, PhD.
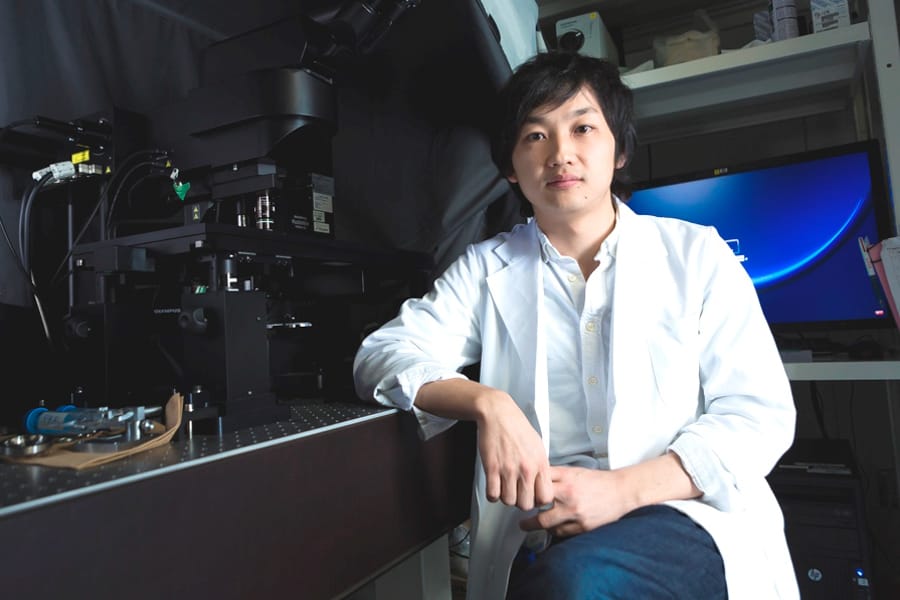
Takanori Takebe, MD (Credit: The New York Stem Cell Foundation)
The scientists who conducted the study, tested their processing system with human organs that had been donated (pancreas, heart, brain, etc.) with induced pluripotent stem cells (iPS). Reprogrammed from a person’s adult cells (like skin cells), iPS cells act like embryonic cells and can form any tissue type in the body.
The tissue-engineering process also uses two types of progenitor cells, which support formation of the body and its specific organs. The progenitor cells are mesenchymal stem cells (MSNs) and human umbilical vascular endothelial cells (HUVECs).
Using donated organ cells, the researchers combined these with MSNs, HUVECs along with other genetic and biochemical material that cue the formation of pancreatic islets. In conditions that nourish and nurture the cells, the ingredients condensed and self-organized into pancreatic islets.
“We need a strategy that ensures successful engraftment through the timely development of vascular networks,” said Taniguchi. “We demonstrate in this study that the self-condensation cell culturing system promotes tissue vascularization.”
Pancreatic islets tissue-engineered in the current generated by the process not only quickly developed a vascular network after transplant into animal models of type 1 diabetes, the tissues also functioned efficiently as part of the endocrine system — secreting hormones like insulin and stabilizing glycemic control in the animals.
Takebe’s and Taniguchi’s research team already have been able to cell culture tissue from liber that can provide a tissue with blood vessels after surgery. Although the ability to create this organ tissue fragments that provide the tissue with blood, was just a goal on the horizon until this study investigators said.
iPSCs vs Adult Stem Cells (MSCs)
This study highlights further use of iPSCs are a valuable research tool. At this time, the methods used to force cells into pluripotency create cells that are dangerous when injected. This makes them unsuitable for therapeutic use, yet perfect for research.
Unlike iPSCs, Dental Pulp Stem Cells (including that of MSCs) do not produce tumours or lesions when transplanted or injected. Multiple studies have shown Dental Pulp Stem Cells to be safe and non-tumor-forming in animals. Dental Pulp Stem Cells have already been used in humans without causing tumors. Additionally, many clinical trials have been completed that show that the use of mesenchymal stem cells from bone marrow in humans is safe.
Protect Their Future Health
If you want more information on how you can protect your child’s future health by banking their cells, get in touch with our friendly team today or order your free information pack.
